Trusts are delivering activity gains in some areas that exceed pre-pandemic levels
The operational asks set out in the planning guidance, the delivery plan for recovering urgent and emergency care, and the elective recovery plan set a number of challenging targets for trusts.
National data shows good early progress towards achieving the interim recovery targets for urgent and emergency care, while in elective services trusts have successfully reduced the number of long waits. However, substantial care backlogs persist across mental health, community, and children and young people’s services.
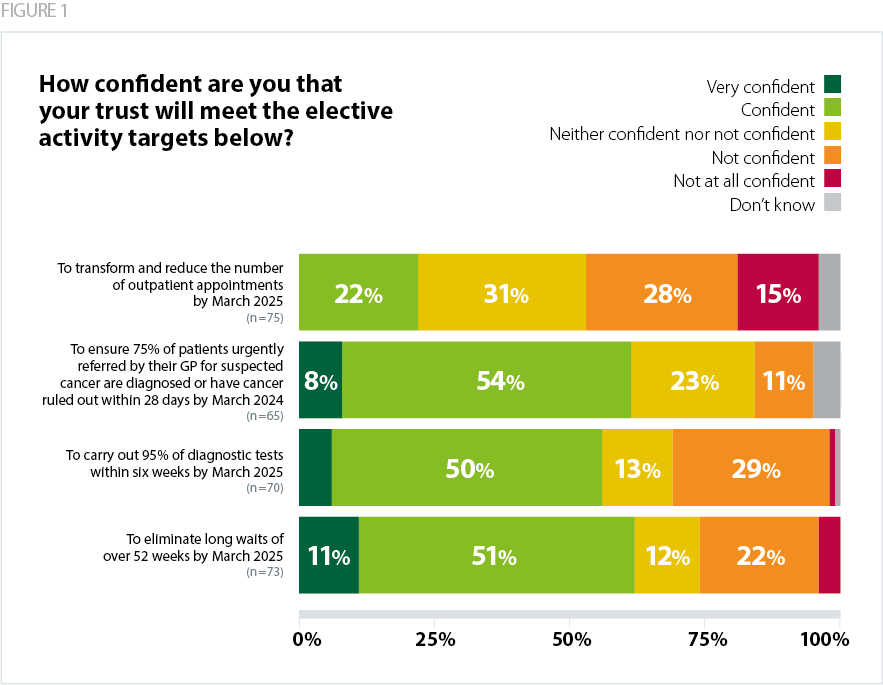
Trust leaders report variable levels of confidence in sustaining progress, as highlighted in the chart below.
Cancer
NHS England’s elective recovery plan set two central targets for cancer care: for 75% of people urgently referred with suspected cancer by their GP to have cancer ruled out or confirmed within 28 days by March 2024; and for the backlog of people waiting over 62 days to start treatment from referral to be brought down to pre-pandemic levels by March 2023.
Our survey results show that nearly two thirds (62%) of trusts were confident they would meet the 28-day diagnosis standard by March 2024. Trusts actually achieved the 28-day standard in February 2023 (NHS England, 2023b). However, the 62-day backlog is still substantially above pre-pandemic levels.
The pandemic severely impacted cancer screening, diagnosis and treatment rates (NHS Digital, 2023b). As a result, demand has increased, and trusts are delivering more tests and treatments than ever. Demand is likely to remain very high, which means it may be difficult to sustain progress.
Diagnostics
Trusts are currently working towards a target of carrying out 95% of diagnostic tests within six weeks by March 2025. Over half (56%) of respondents said they were confident or very confident they would meet the target.
Trusts have delivered record monthly numbers of diagnostic tests in 2023 to date, substantially above pre-pandemic levels. This has been supported by greater investment in community diagnostic centres and new diagnostic equipment.
However, very high levels of demand mean that while trusts have increased activity, progress in working through the backlog has been limited and in March 2023 a quarter (25%) of patients waited over six weeks for a diagnostic test (NHS England, 2023c).
Inpatient and outpatient elective recovery and transformation
In 2022, trusts successfully hit the first elective recovery plan milestone of virtually eliminating all two-year waits for elective care. In the context of historic winter pressures and widespread industrial action, trusts also made strong progress toward the target ofm eliminating 78-week waits by April 2023.
Integrated care systems (ICSs) are also working with trusts toward a target of increasing elective activity to 130% of pre-pandemic levels by 2024/25. However, as we flag in the following section, a range of factors have limited progress. As such, the overall size of the elective backlog has not decreased – as more people join the list, the overall size has exceeded seven million since September 2022 (NHS England, 2023d).
The next milestone in the elective recovery plan is to virtually eliminate 52-week waits by March 2025. Two thirds (62%) of respondents to our survey said they were confident or very confident of hitting this target.
Linked to the elective recovery plan is the ongoing work to transform outpatient services and reduce avoidable follow-up appointments. This is seen as a way to increase capacity and improve productivity in planned care. Trusts are working to reduce outpatient follow-up appointments by 25% compared to 2019/20, though data suggests progress has been very limited (NHS Digital, 2022a). This is reflected in our survey findings, with just over one in five (22%) respondents saying they were confident of achieving the outpatient transformation target.
Urgent and emergency care
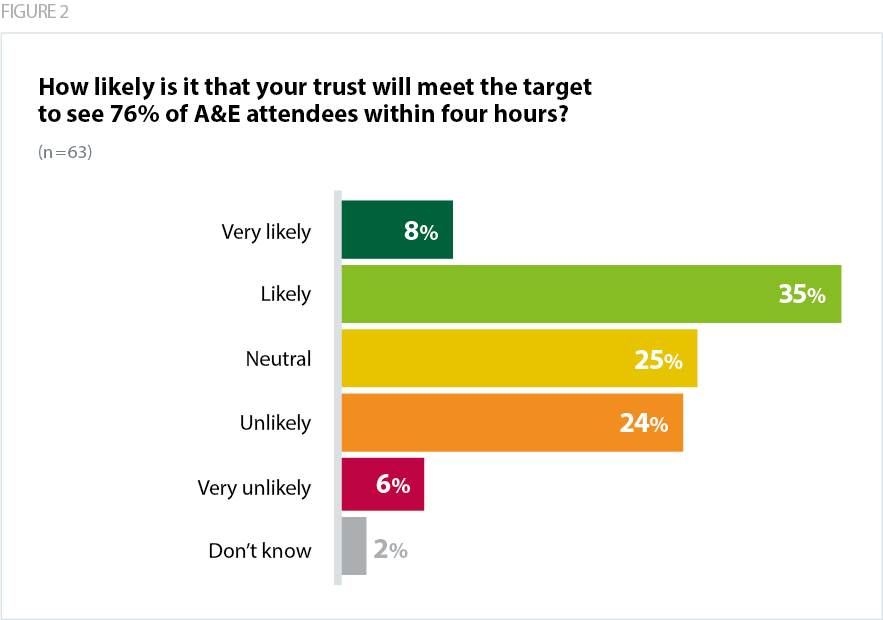
In January 2023, NHS England published the delivery plan for recovering urgent and emergency care services. It set an interim recovery target of 76% of A&E attendances to be seen within four hours over 2023/24 – with further improvements toward the constitutional standard of 95% the following year.
During the winter of 2022/23 performance against the four-hour target hit a record low of 65% (NHS England, 2023e). While the first months of 2023 saw performance improve, this will be a challenging target to achieve, as demand remains high and capacity too low. This is reflected in the fact that fewer than half (43%) of our survey respondents were confident of achieving the target.
One of the key enablers for recovering urgent and emergency care (UEC) performance, highlighted in the recovery plan, is to improve patient flow by increasing capacity across the pathway. The plan set an ambition of reducing average bed capacity to below 92% by creating 5,000 more staffed beds. For context, average bed occupancy across the service was 89.8% in the quarter ending 31 March 2023.
The ambulance sector is also working towards very challenging recovery targets, to improve category two call response times to 30-minutes over the current year, then deliver further improvements the following year. Initial data shows promising early signs but sustaining these gains through the coming months and into winter 2023/24 will be dependent on ensuring extra capacity across UEC pathways.
Mental health and community services
Between 2016/17 and 2021/22 the number of people using NHS mental health services increased from 3.6 million to 4.5 million (NHS Digital, 2023c). Trusts are exploring how best to deliver more mental health care provision in community settings, and the numbers of people accessing treatment has increased. However, the pandemic saw the prevalence of mental health conditions increase, disruption to services and a care backlog develop. There are now an estimated 1.2 million people on waiting lists for community-based NHS mental health services (NAO, 2023).
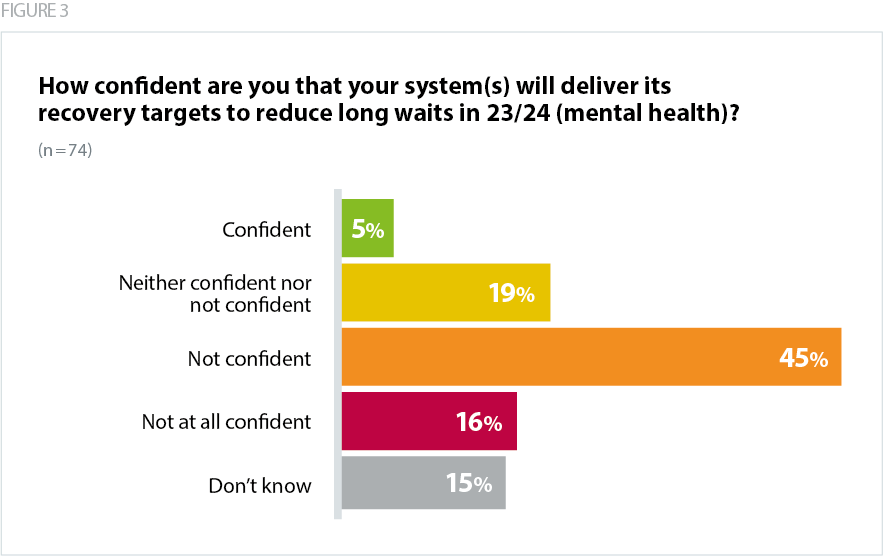
These pressures are reflected in our survey findings, as nearly two thirds (61%) of respondents said they were not confident their system would achieve targets to reduce long waits for mental health care.
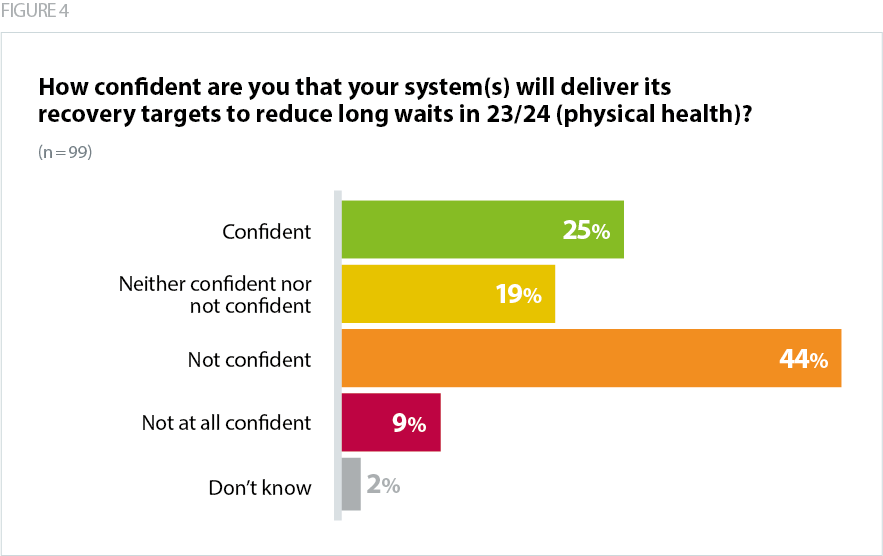
Overall, trust leaders across all sectors are also concerned about making progress in recovering waiting lists for physical health, with over half (53%) of respondents to our survey reporting they were not confident about reducing long waits.
Community service providers are similarly delivering an increasing level of care and taking more referrals. Community providers received 1.5 million referrals in January 2023, a 19% increase on the previous year. In the same month there were 860,000 people waiting to receive community care, a substantial and rising backlog.