Introduction
Today NHS England published its latest weekly situation reports, providing an insight into operational performance across emergency care and hospitals between 12 to 18 February.
The data this week show that demand for urgent and emergency care remains high, despite fewer patients arriving by ambulance in the week to 18 February. The number of patients in hospital with seasonal illnesses such as diarrhoea and vomiting, norovirus and flu, has also fallen slightly this week. However, there are still over a thousand more patients in hospital with flu compared to the same time last year. This is without doubt contributing to the pressures already felt across health and care systems. Challenges with patient flow also persist as a high proportion of patients fit to be discharged remained in hospital. Despite an increase in bed capacity year on year, bed occupancy remains high at 94%.
Winter situation report (12 – 18 February)
A&E closures and diverts: There were no A&E closures this week. There were 25 A&E diverts, three more than the week prior but 21 more than the same time last year.
Ambulance arrivals: A total of 89,377 patients arrived by ambulance in the latest week. This is down by 2% since the week before but up 12.1% compared to the same week last year.
Ambulance handovers: 29.9% of ambulance handovers were delayed by 30 minutes or more, down from 32.6% last week. 12% were delayed by 60 minutes or more, down from 13.3% last week. A total of 23,494 hours were lost to ambulance handover delays, this is 14.6% lower than last week but 36.7% higher than the same week last year.
Critical care: Adult critical care bed occupancy is at 80.2% this week: this is down from 81.4% a week before but is above levels seen in the same week last year (77.7%).
Diarrhoea and vomiting (D&V): There were an average of 607 beds closed due to D&V and norovirus this week, down from 689 last week. This is down by 12% compared to last week and lower than this time last year (821).
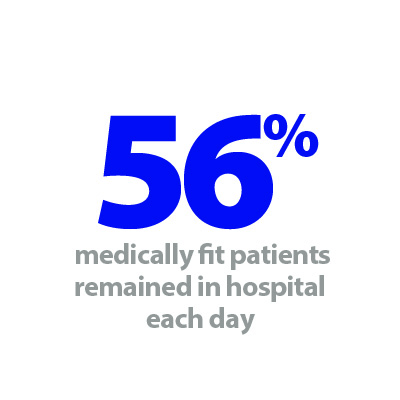
Discharges: On average there were 24,436 patients each day who no longer met the criteria to reside, a slight decrease than the week before (-0.5%). Compared to last week, a smaller proportion of patients remained in hospital (55.8%, or 13,624).
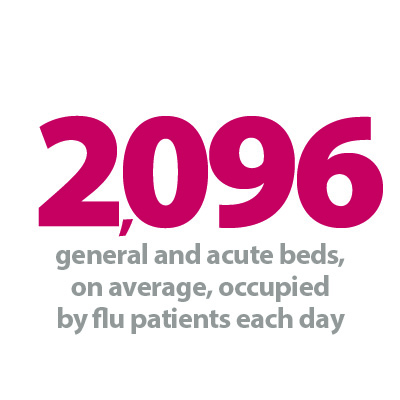
Flu: This week the average number of general and acute beds occupied by flu patients each day decreased by 8.5% to 2,096. This is 3.5 times larger than the same time last year (1,493 more). An average of 112 critical care beds were occupied by flu patients each day this week (14% more than the week before) and 3.2 times greater than same time last year (76 more).
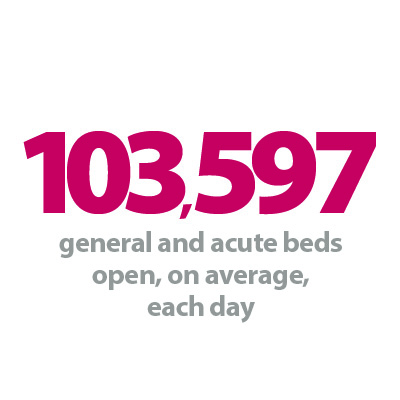
General and acute (G&A) beds: There were an average of 103,597 G&A beds open each day across all acute trusts. On average each day, 71 G&A beds were unavailable and void to non-Covid admissions. Average bed occupancy remains high at 94%. This is up marginally from 93.8% last week but is at a similar level to the same time last year (94.1%).
Long stay: The number of patients staying in hospital longer than 21 days increased slightly this week (+0.6%). However, those staying longer than seven and 14 days decreased by 0.6% and 0.2% respectively.
Neonatal intensive care beds: For all trusts, bed occupancy is now at 69.7%, staying at a similar level to last week (69.6%). This is up from 66.7% the same week a year before. The average number of care beds open is at 1,720, 17 more beds open compared to the same time last year.
Paediatric intensive care beds: For all trusts, bed occupancy has decreased this week to 77.5%, down from 77.9% last week. The average number of paediatric intensive care beds open this week has fallen by one to 372.
Respiratory syncytial virus (RSV): An average of 11 paediatric beds were closed this week due to RSV symptoms, down from 18 last week and down from 16 last year.
Staff absences: There were an average of 46,834 total absences each day this week, of which 3% were Covid-19 related (1,236). The total number of staff absences decreased from the week before (48,482) but the proportion of Covid-19 related absences was the same.
Our view
The data this week continues to highlight the extent of the pressures being felt across NHS services. Demand for urgent and emergency care remains a cause of concern as the numbers of patients arriving in hospital by ambulance remains higher than this time last year. Furthermore, despite seeing improvements in December, the total number of hours lost to ambulance handover delays in February also remains considerably higher than levels observed last year.
Patient flow also remains a significant challenge for systems, as over half of patients (55.8%), who were medically fit to be discharged remained in hospital. This equates to almost 14,000 beds being taken up every day by patients who are fit to leave but cannot. Trust leaders tell us that the reasons driving delayed discharges are multifaceted. However, they are, in part, due to the increased complexity of patients they are treating, alongside ongoing capacity pressures in social care.
General and acute bed occupancy also remains high at 94% despite the addition of more beds since last year. Encouragingly, the data show another fall in paediatric intensive care unit bed occupancy compared to last week, while patients staying in hospital for longer than seven and 14 days has fallen. However, with high levels of ambulance callouts, high bed occupancy and persistent winter viruses, winter pressures do not yet appear to be easing overall.
With further industrial action set to take place this week, it is important that the government and unions work together to find a resolution so staff can continue to work towards tackling the care waiting lists and providing patients with high quality care.
Clinical hubs benefitting patients and reducing demand on A&E
For this week's NHS Winter Watch campaign, we take a look at how clinical hubs set up by South East Coast Ambulance Service NHS Foundation Trust (SECAmb) are benefitting patients and reducing demand on A&E.
Two clinical co-ordination hubs set up as trials by SECAmb, in partnership with NHS trusts in Kent, have been extended having delivered positive early results.
The hubs, established in autumn last year, in the trust's Paddock Wood and Ashford operational areas, involve multi-discipline teams from across the Kent healthcare system joining SECAmb paramedic practitioners to ensure 999 calls are receiving the most appropriate response. By reviewing appropriate 999 calls, the hubs are helping to reduce pressure on A&E by guiding patients to the most appropriate service and supporting ambulance crews at the scene of an incident.
Based at the trust's Ashford and Paddock Wood Make Ready Centres, SECAmb teams are joined by emergency department consultants and clinicians from East Kent Hospitals University NHS Foundation Trust, Maidstone and Tunbridge Wells NHS Trust and urgent care teams, including the home treatment service at Kent Community Health NHS Foundation Trust.
In the 15 weeks since the beginning of October last year, the West Kent clinical coordination hub has made more than 1,400 contacts with crews and discharged more than 200 patients on scene. It has helped avoid conveyance to an emergency department for more than 500 patients where the original plan was to convey; supported 79 medical Same Day Emergency Care (SDEC) referrals and 19 surgical SDEC referrals; arranged 90 GP in emergency department appointments; and referred 191 patients directly into a home treatment team.
The Ashford Integrated Care Hub has enjoyed similar success since its launch at the beginning of November 2023. Over the last three months it has made more than 1,500 contacts with ambulance crews and discharged more than 600 patients on scene. It has also arranged more appropriate care for more than 800 patients who were due to attend an emergency department. The hub has supported more than 100 medical SDEC referrals and more than 100 urgent community response referrals. Some 180 GP in emergency department appointments have been arranged and the team has referred approximately 250 patients directly into a home treatment team.
SECAmb operations manager for Ashford, Nakai Redman said: "The first three months the hub has been in operation have been extremely encouraging. The results have shown that by having a multi-discipline approach to reviewing 999 calls, we can improve the response and ultimately the care we provide the local community.
"We have also seen a significant improvement in work satisfaction from colleagues as they are finding they are more often being sent to emergencies where they can make a difference and help patients with the support of shared decision making."
SECAmb practice development lead and the trust's lead at the Paddock Wood hub, Sean Edwards said: "Our clinical coordination hub is a true collaboration between acute and community services that is directly benefitting patients, ensuring they can be seen in the right place, first time for their condition, and reducing unnecessary emergency department attendances. Furthermore, ambulance crews have access to senior clinicians to aid in complex decision making, ensuring patient safety and improving the quality of care we can provide our patients in West Kent."